Sperm donation is the name of the practice by which a man, known as a sperm donor, provides his semen with the intention that it be used to produce a baby where the man does not have sexual relations with the recipient of his semen. Attempts are made to impregnate a woman with the donor's sperm using third party reproduction techniques notably artificial insemination.
A sperm donor may donate his sperm directly to the woman recipient, or he may donate it at a clinic known as a sperm bank.
Sperm donation commonly assists couples unable to produce children because of 'male factor' fertility problems,[citation needed] but it is increasingly used as a means to enable single women and single and coupled lesbians to have their own children.[citation needed] The sperm donor is the genetic or biological father of each child produced with the use of his sperm. When a donor's sperm is successfully used repeatedly for impregnation, numbers of siblings and half-siblings will be produced.
Donors may be either anonymous or non-anonymous, although laws may require donors to be one or the other, or restrict the number of children each donor may father. Although many donors choose to remain anonymous, new technologies such as the internet and DNA technology has opened up new avenues for those wishing to know more about the biological father, siblings and half-siblings.
Process
When a sperm donor provides his sperm through a sperm bank or fertility clinic he will usually enter into a contract to donate sperm for a specified contractual minimum period of time ranging from six to twenty four months. To donate sperm a man must generally meet specific requirements regarding age and medical history. In the United States, sperm banks are regulated as Human Cell and Tissue or Cell and Tissue Bank Product (HCT/Ps) establishments by the FDA. Many states also have regulations in addition to those imposed by the FDA. A man generally donates sperm at a clinic or sperm bank by way of masturbation in a private room or cabin, known as a 'men's production room' (UK) or a 'masturbatorium' (USA). Many of these facilities contain pornography such as videos, magazines, and/or photographs in order to assist the donor to produce the ejaculate.
Types of donors
General
This section does not cite any references or sources.
Please help improve this section by adding citations to reliable sources. Unverifiable material may be challenged and removed. (January 2008)
Many sperm donors donate their sperm for purely altruistic reasons so that childless women or couples may produce their own children.[citation needed] Where such donations are through a sperm bank, the sperm bank will generally re-imburse the donor his reasonable expenses.[citation needed]
Some sperm donors may however, seek financial compensation, particularly those who supply sperm samples to order at specific times and at a specific sperm bank on a regular basis for what may be many months, in the knowledge that these samples will be used to produce a number of pregnancies. Many sperm banks therefore offer financial rewards which more adequately compensate for such a commitment.[citation needed] A sperm donor will rarely, if ever, know the exact number of pregnancies which his samples have produced, and indeed, an accurate or exact figure very often will not exist.[citation needed]
In the past sperm banks were keen to recruit as sperm donors men who had already fathered children. However, with the advances of microbiology, sperm can readily be checked for its fecundity, and sperm banks will now rely upon their own tests to ensure the quality of sperm.
Sperm donors are required to be fit and healthy and generally their 'sperm count' will be well above average to ensure that pregnancies may be easily and swiftly achieved by the use of their sperm. Sperm banks impose age restrictions on donors, usually from 18 to 40 or 45, but in practice the majority of donors are young men who are often college students.[citation needed]
Donated sperm may be prepared for use by artificial insemination in intrauterine insemination (ICI) or intra-cervical insemination (ICI), or it may be prepared for use through other assisted reproduction techniques (ART). Donated sperm may also be used in surrogacy arrangements and for producing embryos with donated eggs for implanting in a woman who is not genetically related to the child she produces and who may or may not be a surrogate.
Sperm banks maintain lists or catalogues of donors which provide basic information about the donor such as racial origin, height, weight, colour of eyes, blood group etc. Some of these catalogues are available for browsing via the internet, whilst others are only made available to patients when they apply to a sperm bank for treatment. Some sperm banks make additional information about each donor available for an additional fee, and others make additional basic information known to children prodcued from donors when those children reach the age of eighteen. Some clinics offer 'exclusive donors' whose sperm is only used to produce pregnancies for one recipient woman. How accurate this is, or can be, is not known, and neither is it known whether the information produced by sperm banks, or by the donors themseles, is true. Many sperm banks will, however carry out whatever checks they can to verify the information they request, such as checking the identity of the donor and contacting his own doctor to verify medical details. Simply because such information is not verifiable does not imply that it is in any way inaccurate, and a sperm bank will rely upon its reputation which, in turn, will be based upon its success rate and upon the accuracy of the information about its donors which it makes available.
Anonymous or non-anonymous
Anonymous sperm donation is where the child and/or receiving couple will never get to know the identity of the donor, and non-anonymous when they will.
A donor who makes a non-anonymous sperm donation is termed a known donor.
Anonymous
Most sperm donors are anonymous, i.e. the clinic will never give contact information of the receiving woman/couple and the woman/couple will not be told the identity of the donor. However some information about the donor may be released to the woman/couple. A limited donor information at most includes height, weight, eye, skin and hair colour. In Sweden, this is all the information a receiver gets. In the US, on the other hand, additional information may be given, such as a comprehensive biography and sound/video samples.
The law usually protects sperm donors from being responsible for children produced from their donations, and the law also usually provides that sperm donors have no rights over the children which they produce.
Non-anonymous
Several countries, e.g. Sweden, Norway, the Netherlands, Britain, Switzerland, Australia[1] and New Zealand only allow non-anonymous sperm donation. The child may, when grown up (15-18 years old), get contact information from the sperm bank about his/her biological father. In Denmark, however, a sperm donor may choose to be either anonymous or non-anonymous. Nevertheless, the initial information which the receiving woman/couple will receive is the same. In the United States, sperm banks are permitted to disclose the identity of a non-anonymous donor to any children brought to the world by that donor, once the child turns 18.[2]
Private donors
Besides the men who donate to a sperm bank there are also less institutional donations. For example, mother may approach a friend, or may obtain a "private" donor by advertising. A number of web sites seek to link such donors and donees, while advertisements in same sex publications are not uncommon. Although artificial insemination is usually used, frozen sperm need not be. Most such donors meet the donees and are therefore usually known to the recipient. Private donations are usually free - avoiding the significant costs of a more medicalised insemination - and theoretically, where fresh rather than frozen semen is used the chances of pregnancy may be higher. Against this are the usually higher risks of disease transmission and the risk of a legal dispute regarding access or maintenance. The laws of some nations (e.g. New Zealand), allow for recognition of written agreements between donors and donees in a similar way to institutional donations. In others, e.g. Sweden[3], this is not guaranteed.
Limitation
Where a sperm donor donates sperm through a sperm bank, the sperm bank will generally undertake a number of medical and scientific checks to ensure that the donor produces sperm of sufficient quantity and quality and that the donor is healthy and will not pass diseases through the use of his sperm. The donor's sperm must also withstand the freezing and thawing process necessary to store and quarantine the sperm. The cost to the sperm bank for such tests is not inconsiderable. This normally means that clinics may use the same donor to produce a number of pregnancies in a number of different women.
A sperm donor generally enters into an agreement with the sperm bank to supply sperm usually once a week for a period of between four months and two years, depending on the extent to which the sperm may be used to produce the maximum number of pregnancies permitted (if any)(but see also below, "Onselling"). A single donation (i.e. one ejaculate) prepared into samples for intra-cervical use (ICI) or a donation prepared into 'washed' samples for intrauterine insemination (IUI) will enable each sample to have about the same chance of producing a pregnancy as sperm delivered through sexual intercourse (i.e. a rate of btween 7 and 20% depending on a number of factors). Samples prepared for other ART uses may allow more pregnancies to be produced from one donation. A single donation prepared into samples for IVF for example, may be sufficient to fertilise up to eight batches of eggs. The success rate for embryos subsequently implanted in a woman is approximately between 20 and 45% per treatment cycle (see assisted reproduction). 'Washed' or 'unwashed' samples may also be used for ICSI thus increasing the number of pregnancies produced from a single donation.
The number of children permitted to be born from a single donor varies according to law and practice. Laws vary from state to state, and a sperm bank may also impose its own limits. The latter will be based on the reports of pregnancies which the sperm bank receives, although this relies upon the accuracy of the returns and the actual number of pregnancies may therefore be somewhat higher. Nevertheless, sperm banks frequently impose a lower limit on geographical numbers than some US states and may also limit the overall number of pregnancies which are permitted from a single donor. When calculating the numbers of children born from each donor, the number of siblings produced in any 'family' as a result of sperm donation from the same donor are almost always excluded (but see below for the provisions in various states). There is, of course, no limit to the number of offspring which may be produced from a single donor where he supplies his sperm privately.
Where a limit on the number of offspring which are allowed to be produced from each donor is imposed, this is usually in order to reduce the chance of consanguinity by the half-siblings of the donor. However, some donors may produce substantial numbers of offspring, particularly where they donate through different clinics, where sperm is onsold or is exported to different jurisdictions, and where countries or states do not have a central register of donors.
Sperm banks frequently publish their 'pregnancy rates' which are success rates according to the number of pregnancies achieved as a percentage of the total number of treatments provided. Sperm banks may also publish 'birth rates' giving the number of live births as a percentage of treatment cycles. These rates vary from clinic to clinic, according to the method of insemination or ART used and of the ages of the recipients. Sperm from a sperm donor may be used by a clinic until the maximum number (if any) of live births in each case has been achieved.
Sperm may also be donated through an agency rather than through a sperm bank. The agency recruits sperm donors, usually via the internet, and it also advertises its services on the internet. Donors undergo the same kind of checks and tests required by a sperm bank. However, in the case of an agency, the sperm will be supplied to the recipient woman fresh rather than frozen. A woman chooses a donor and notifies the agency when she requires donations. The agency notifies the donor who supplies his sperm on the appropriate days in a container provided by the agency. This is collected and delivered by courier and the woman uses the donor's sperm to perform her own insemination. The whole process preserves the anonymity of the parties but it is largely unregulated and, because the sperm is not quarantined, it carries risks which are not associated with sperm banks. Donors providing sperm in this way will not be protected by laws which apply to donations through a sperm bank or fertility clinic and will, if traced, be regarded as the legal father of each child produced by their sperm. In addition, agencies rarely impose or enforce limits on the numbers of children which may be produced by a particular donor.
Onselling
There is a market for vials of processed sperm and for various reasons a sperm bank may sell on stocks of vials which it holds (known as 'onselling'). Onselling therefore enables a sperm bank to maximize the sale and disposal of sperm samples which it has processed. The reasons for onselling may be where part of, or even the main business of, a particular sperm bank is to process and store sperm rather than to use it in fertility treatments, or where a sperm bank is able to collect and store more sperm than it can use within nationally set limits. In the latter case a sperm bank may sell on sperm from a particular donor for use in another jurisdiction after the number of pregnancies achieved from that donor has reached its national maximum..
A UK sperm bank however, may only onsell sperm before the national limit of ten families has been achieved from one donor within the UK. This means, for example, that a sperm bank may recruit a donor and prepare samples for ICI, IUI and ART use from his donations. After 9 months it is able to release the 10 or so samples donated within the first 3 months, from 6 month quarantine ( approximately 100 vials) and it uses these to achieve 6 pregnancies (although more pregnancies could, of course, be achieved from the number of vials prepared as illustrated). The sperm bank is then able to onsell sperm from that donor to sperm banks and clinics outside the UK and it can illustrate the fecundity of the various types of samples it sells. The donor may continue to donate for several years (usually 3 or 4) and the UK clinic will be able to achieve a further 4 pregnancies in the UK at the end of that period within the UK rules. It will also continue to hold stocks of that donor's sperm for sibling use after that time. The donor must however, have agreed to the export and to the use of his donations abroad, and he must be told that reguations for use outside the UK will vary. He must not have put a limit on the number of births which may be achieved from his donations. The HFEA must be notified of exports of sperm from the UK but it does not limit these since it is only concerned with the storage and use of sperm within the UK.
Emrbyos may also be onsold. In the case of the UK, because the embryo wll have been created in the UK under a regulated process, the consent of the HFEA must be obtained if these are to be exported.
Onselling is normally only appropriate where the donor remains anonymous. Sperm banks purchasing sperm samples may in turn onsell these to other sperm banks. Onselling may therefore give rise to numerous pregnancies being produced from individual donors, but in every case rules as to use and the limitation on the number of pregnacies which apply locally will reduce the risk of consanguinity. The lack of overall records as to use and success will mean that the numbers of pregnancies achieved from the samples of an individual donor will not exist and the donor will not be at risk of knowing the large number of births that were produced from the samples he donated.
Sperm may also be sold on for research or educational purposes, usually after the number of births from the donor concerned has reached its maximum. Sperm is used for genetic and fertility testing, and also for research into birth control.
Donor tracking
Even when the donor had chosen to be anonymous, there are still opportunities to find the biological father for curious people conceived by donor sperm. Registries and DNA-databases are useful for this purpose.
Tracking by registries
Some donors are non-anonymous, but most are anonymous, i.e. the donor conceived person doesn't know the true identity of the donor. Still, he/she may get the donor number from the fertility clinic. If that donor had donated before, then other donor conceived people with the same donor number are thus genetic half-siblings. In short, donor registries matches people who type in the same donor number.
Tracking by DNA-databases
However, even sperm donors who have not initiated contact through a registry are now increasingly being traced by their offspring. In the current era there can be no such thing as guaranteed anonymity. Through the advent of DNA testing and internet access to extensive databases of information, one sperm donor has recently been traced. In 2005 it was revealed in New Scientist magazine[4] that an enterprising 15-year-old used information from a DNA test and the internet to identify and contact his genetic father, who was a sperm donor. This has brought into question the ability of sperm donors to stay anonymous.
Payment
The majority of sperm donors who donate their sperm through a sperm bank receive some kind of payment. This varies from the situation in the United Kingdom where donors are only entitled to their expenses in connection with the donation, to the situation with some US sperm banks where a donor receives a set fee for each donation plus an additional amount for each vial stored. Whilst the amounts concerned in each case are not excessive, some donors are known to donate to more than one sperm bank every week and they are thus able to secure a reasonable monthly income.
Some private donors may seek remuneration although the majority of these donate for altruistic reasons. Equipment to collect, freeze and store sperm is available to the public notably through certain US outlets, and some donors process and store their own sperm which they then sell via the internet.
The selling price of processed and stored sperm is considerably more than the sums which are received by donors. Treatments with donor sperm are generally expensive and are seldom available free of charge through national health services. Sperm banks often package treatments into eg three cycles, and in cases of IVF or other ART treatments, they may reduce the charge if a patient donates any spare embryos which are produced through the treatment. There is often more demand for fertiltity treatment with donor sperm than there is donor sperm available, and this has the effect of keeping the cost of such treatments reasonably high.
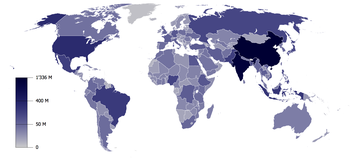
International comparison
On the global market, Denmark has a well developed system of sperm export. This success mainly comes from the reputation of Danish sperm donors for being of high quality and, in contrast with the law in the other Nordic countries, gives donors the choice to remain anonymous to the receiving couple.[5] However, they supply non-anonymous samples as well. More than 50 countries worldwide are importers, including Paraguay, Canada, Kenya and Hong Kong.[5] However, the Food and Drug Administration (FDA) of the US has banned import of any sperm, motivated by a risk of mad cow disease.[6]
A sperm donor may donate his sperm directly to the woman recipient, or he may donate it at a clinic known as a sperm bank.
Sperm donation commonly assists couples unable to produce children because of 'male factor' fertility problems,[citation needed] but it is increasingly used as a means to enable single women and single and coupled lesbians to have their own children.[citation needed] The sperm donor is the genetic or biological father of each child produced with the use of his sperm. When a donor's sperm is successfully used repeatedly for impregnation, numbers of siblings and half-siblings will be produced.
Donors may be either anonymous or non-anonymous, although laws may require donors to be one or the other, or restrict the number of children each donor may father. Although many donors choose to remain anonymous, new technologies such as the internet and DNA technology has opened up new avenues for those wishing to know more about the biological father, siblings and half-siblings.
Process
When a sperm donor provides his sperm through a sperm bank or fertility clinic he will usually enter into a contract to donate sperm for a specified contractual minimum period of time ranging from six to twenty four months. To donate sperm a man must generally meet specific requirements regarding age and medical history. In the United States, sperm banks are regulated as Human Cell and Tissue or Cell and Tissue Bank Product (HCT/Ps) establishments by the FDA. Many states also have regulations in addition to those imposed by the FDA. A man generally donates sperm at a clinic or sperm bank by way of masturbation in a private room or cabin, known as a 'men's production room' (UK) or a 'masturbatorium' (USA). Many of these facilities contain pornography such as videos, magazines, and/or photographs in order to assist the donor to produce the ejaculate.
Types of donors
General
This section does not cite any references or sources.
Please help improve this section by adding citations to reliable sources. Unverifiable material may be challenged and removed. (January 2008)
Many sperm donors donate their sperm for purely altruistic reasons so that childless women or couples may produce their own children.[citation needed] Where such donations are through a sperm bank, the sperm bank will generally re-imburse the donor his reasonable expenses.[citation needed]
Some sperm donors may however, seek financial compensation, particularly those who supply sperm samples to order at specific times and at a specific sperm bank on a regular basis for what may be many months, in the knowledge that these samples will be used to produce a number of pregnancies. Many sperm banks therefore offer financial rewards which more adequately compensate for such a commitment.[citation needed] A sperm donor will rarely, if ever, know the exact number of pregnancies which his samples have produced, and indeed, an accurate or exact figure very often will not exist.[citation needed]
In the past sperm banks were keen to recruit as sperm donors men who had already fathered children. However, with the advances of microbiology, sperm can readily be checked for its fecundity, and sperm banks will now rely upon their own tests to ensure the quality of sperm.
Sperm donors are required to be fit and healthy and generally their 'sperm count' will be well above average to ensure that pregnancies may be easily and swiftly achieved by the use of their sperm. Sperm banks impose age restrictions on donors, usually from 18 to 40 or 45, but in practice the majority of donors are young men who are often college students.[citation needed]
Donated sperm may be prepared for use by artificial insemination in intrauterine insemination (ICI) or intra-cervical insemination (ICI), or it may be prepared for use through other assisted reproduction techniques (ART). Donated sperm may also be used in surrogacy arrangements and for producing embryos with donated eggs for implanting in a woman who is not genetically related to the child she produces and who may or may not be a surrogate.
Sperm banks maintain lists or catalogues of donors which provide basic information about the donor such as racial origin, height, weight, colour of eyes, blood group etc. Some of these catalogues are available for browsing via the internet, whilst others are only made available to patients when they apply to a sperm bank for treatment. Some sperm banks make additional information about each donor available for an additional fee, and others make additional basic information known to children prodcued from donors when those children reach the age of eighteen. Some clinics offer 'exclusive donors' whose sperm is only used to produce pregnancies for one recipient woman. How accurate this is, or can be, is not known, and neither is it known whether the information produced by sperm banks, or by the donors themseles, is true. Many sperm banks will, however carry out whatever checks they can to verify the information they request, such as checking the identity of the donor and contacting his own doctor to verify medical details. Simply because such information is not verifiable does not imply that it is in any way inaccurate, and a sperm bank will rely upon its reputation which, in turn, will be based upon its success rate and upon the accuracy of the information about its donors which it makes available.
Anonymous or non-anonymous
Anonymous sperm donation is where the child and/or receiving couple will never get to know the identity of the donor, and non-anonymous when they will.
A donor who makes a non-anonymous sperm donation is termed a known donor.
Anonymous
Most sperm donors are anonymous, i.e. the clinic will never give contact information of the receiving woman/couple and the woman/couple will not be told the identity of the donor. However some information about the donor may be released to the woman/couple. A limited donor information at most includes height, weight, eye, skin and hair colour. In Sweden, this is all the information a receiver gets. In the US, on the other hand, additional information may be given, such as a comprehensive biography and sound/video samples.
The law usually protects sperm donors from being responsible for children produced from their donations, and the law also usually provides that sperm donors have no rights over the children which they produce.
Non-anonymous
Several countries, e.g. Sweden, Norway, the Netherlands, Britain, Switzerland, Australia[1] and New Zealand only allow non-anonymous sperm donation. The child may, when grown up (15-18 years old), get contact information from the sperm bank about his/her biological father. In Denmark, however, a sperm donor may choose to be either anonymous or non-anonymous. Nevertheless, the initial information which the receiving woman/couple will receive is the same. In the United States, sperm banks are permitted to disclose the identity of a non-anonymous donor to any children brought to the world by that donor, once the child turns 18.[2]
Private donors
Besides the men who donate to a sperm bank there are also less institutional donations. For example, mother may approach a friend, or may obtain a "private" donor by advertising. A number of web sites seek to link such donors and donees, while advertisements in same sex publications are not uncommon. Although artificial insemination is usually used, frozen sperm need not be. Most such donors meet the donees and are therefore usually known to the recipient. Private donations are usually free - avoiding the significant costs of a more medicalised insemination - and theoretically, where fresh rather than frozen semen is used the chances of pregnancy may be higher. Against this are the usually higher risks of disease transmission and the risk of a legal dispute regarding access or maintenance. The laws of some nations (e.g. New Zealand), allow for recognition of written agreements between donors and donees in a similar way to institutional donations. In others, e.g. Sweden[3], this is not guaranteed.
Limitation
Where a sperm donor donates sperm through a sperm bank, the sperm bank will generally undertake a number of medical and scientific checks to ensure that the donor produces sperm of sufficient quantity and quality and that the donor is healthy and will not pass diseases through the use of his sperm. The donor's sperm must also withstand the freezing and thawing process necessary to store and quarantine the sperm. The cost to the sperm bank for such tests is not inconsiderable. This normally means that clinics may use the same donor to produce a number of pregnancies in a number of different women.
A sperm donor generally enters into an agreement with the sperm bank to supply sperm usually once a week for a period of between four months and two years, depending on the extent to which the sperm may be used to produce the maximum number of pregnancies permitted (if any)(but see also below, "Onselling"). A single donation (i.e. one ejaculate) prepared into samples for intra-cervical use (ICI) or a donation prepared into 'washed' samples for intrauterine insemination (IUI) will enable each sample to have about the same chance of producing a pregnancy as sperm delivered through sexual intercourse (i.e. a rate of btween 7 and 20% depending on a number of factors). Samples prepared for other ART uses may allow more pregnancies to be produced from one donation. A single donation prepared into samples for IVF for example, may be sufficient to fertilise up to eight batches of eggs. The success rate for embryos subsequently implanted in a woman is approximately between 20 and 45% per treatment cycle (see assisted reproduction). 'Washed' or 'unwashed' samples may also be used for ICSI thus increasing the number of pregnancies produced from a single donation.
The number of children permitted to be born from a single donor varies according to law and practice. Laws vary from state to state, and a sperm bank may also impose its own limits. The latter will be based on the reports of pregnancies which the sperm bank receives, although this relies upon the accuracy of the returns and the actual number of pregnancies may therefore be somewhat higher. Nevertheless, sperm banks frequently impose a lower limit on geographical numbers than some US states and may also limit the overall number of pregnancies which are permitted from a single donor. When calculating the numbers of children born from each donor, the number of siblings produced in any 'family' as a result of sperm donation from the same donor are almost always excluded (but see below for the provisions in various states). There is, of course, no limit to the number of offspring which may be produced from a single donor where he supplies his sperm privately.
Where a limit on the number of offspring which are allowed to be produced from each donor is imposed, this is usually in order to reduce the chance of consanguinity by the half-siblings of the donor. However, some donors may produce substantial numbers of offspring, particularly where they donate through different clinics, where sperm is onsold or is exported to different jurisdictions, and where countries or states do not have a central register of donors.
Sperm banks frequently publish their 'pregnancy rates' which are success rates according to the number of pregnancies achieved as a percentage of the total number of treatments provided. Sperm banks may also publish 'birth rates' giving the number of live births as a percentage of treatment cycles. These rates vary from clinic to clinic, according to the method of insemination or ART used and of the ages of the recipients. Sperm from a sperm donor may be used by a clinic until the maximum number (if any) of live births in each case has been achieved.
Sperm may also be donated through an agency rather than through a sperm bank. The agency recruits sperm donors, usually via the internet, and it also advertises its services on the internet. Donors undergo the same kind of checks and tests required by a sperm bank. However, in the case of an agency, the sperm will be supplied to the recipient woman fresh rather than frozen. A woman chooses a donor and notifies the agency when she requires donations. The agency notifies the donor who supplies his sperm on the appropriate days in a container provided by the agency. This is collected and delivered by courier and the woman uses the donor's sperm to perform her own insemination. The whole process preserves the anonymity of the parties but it is largely unregulated and, because the sperm is not quarantined, it carries risks which are not associated with sperm banks. Donors providing sperm in this way will not be protected by laws which apply to donations through a sperm bank or fertility clinic and will, if traced, be regarded as the legal father of each child produced by their sperm. In addition, agencies rarely impose or enforce limits on the numbers of children which may be produced by a particular donor.
Onselling
There is a market for vials of processed sperm and for various reasons a sperm bank may sell on stocks of vials which it holds (known as 'onselling'). Onselling therefore enables a sperm bank to maximize the sale and disposal of sperm samples which it has processed. The reasons for onselling may be where part of, or even the main business of, a particular sperm bank is to process and store sperm rather than to use it in fertility treatments, or where a sperm bank is able to collect and store more sperm than it can use within nationally set limits. In the latter case a sperm bank may sell on sperm from a particular donor for use in another jurisdiction after the number of pregnancies achieved from that donor has reached its national maximum..
A UK sperm bank however, may only onsell sperm before the national limit of ten families has been achieved from one donor within the UK. This means, for example, that a sperm bank may recruit a donor and prepare samples for ICI, IUI and ART use from his donations. After 9 months it is able to release the 10 or so samples donated within the first 3 months, from 6 month quarantine ( approximately 100 vials) and it uses these to achieve 6 pregnancies (although more pregnancies could, of course, be achieved from the number of vials prepared as illustrated). The sperm bank is then able to onsell sperm from that donor to sperm banks and clinics outside the UK and it can illustrate the fecundity of the various types of samples it sells. The donor may continue to donate for several years (usually 3 or 4) and the UK clinic will be able to achieve a further 4 pregnancies in the UK at the end of that period within the UK rules. It will also continue to hold stocks of that donor's sperm for sibling use after that time. The donor must however, have agreed to the export and to the use of his donations abroad, and he must be told that reguations for use outside the UK will vary. He must not have put a limit on the number of births which may be achieved from his donations. The HFEA must be notified of exports of sperm from the UK but it does not limit these since it is only concerned with the storage and use of sperm within the UK.
Emrbyos may also be onsold. In the case of the UK, because the embryo wll have been created in the UK under a regulated process, the consent of the HFEA must be obtained if these are to be exported.
Onselling is normally only appropriate where the donor remains anonymous. Sperm banks purchasing sperm samples may in turn onsell these to other sperm banks. Onselling may therefore give rise to numerous pregnancies being produced from individual donors, but in every case rules as to use and the limitation on the number of pregnacies which apply locally will reduce the risk of consanguinity. The lack of overall records as to use and success will mean that the numbers of pregnancies achieved from the samples of an individual donor will not exist and the donor will not be at risk of knowing the large number of births that were produced from the samples he donated.
Sperm may also be sold on for research or educational purposes, usually after the number of births from the donor concerned has reached its maximum. Sperm is used for genetic and fertility testing, and also for research into birth control.
Donor tracking
Even when the donor had chosen to be anonymous, there are still opportunities to find the biological father for curious people conceived by donor sperm. Registries and DNA-databases are useful for this purpose.
Tracking by registries
Some donors are non-anonymous, but most are anonymous, i.e. the donor conceived person doesn't know the true identity of the donor. Still, he/she may get the donor number from the fertility clinic. If that donor had donated before, then other donor conceived people with the same donor number are thus genetic half-siblings. In short, donor registries matches people who type in the same donor number.
Tracking by DNA-databases
However, even sperm donors who have not initiated contact through a registry are now increasingly being traced by their offspring. In the current era there can be no such thing as guaranteed anonymity. Through the advent of DNA testing and internet access to extensive databases of information, one sperm donor has recently been traced. In 2005 it was revealed in New Scientist magazine[4] that an enterprising 15-year-old used information from a DNA test and the internet to identify and contact his genetic father, who was a sperm donor. This has brought into question the ability of sperm donors to stay anonymous.
Payment
The majority of sperm donors who donate their sperm through a sperm bank receive some kind of payment. This varies from the situation in the United Kingdom where donors are only entitled to their expenses in connection with the donation, to the situation with some US sperm banks where a donor receives a set fee for each donation plus an additional amount for each vial stored. Whilst the amounts concerned in each case are not excessive, some donors are known to donate to more than one sperm bank every week and they are thus able to secure a reasonable monthly income.
Some private donors may seek remuneration although the majority of these donate for altruistic reasons. Equipment to collect, freeze and store sperm is available to the public notably through certain US outlets, and some donors process and store their own sperm which they then sell via the internet.
The selling price of processed and stored sperm is considerably more than the sums which are received by donors. Treatments with donor sperm are generally expensive and are seldom available free of charge through national health services. Sperm banks often package treatments into eg three cycles, and in cases of IVF or other ART treatments, they may reduce the charge if a patient donates any spare embryos which are produced through the treatment. There is often more demand for fertiltity treatment with donor sperm than there is donor sperm available, and this has the effect of keeping the cost of such treatments reasonably high.
International comparison
On the global market, Denmark has a well developed system of sperm export. This success mainly comes from the reputation of Danish sperm donors for being of high quality and, in contrast with the law in the other Nordic countries, gives donors the choice to remain anonymous to the receiving couple.[5] However, they supply non-anonymous samples as well. More than 50 countries worldwide are importers, including Paraguay, Canada, Kenya and Hong Kong.[5] However, the Food and Drug Administration (FDA) of the US has banned import of any sperm, motivated by a risk of mad cow disease.[6]


No comments:
Post a Comment